Meeting the Needs of Spinal Cord Injured Armed Forces

Sharon Wood, a Clinical Nurse Specialist in Neuro Urology and Sexual Health, discusses the important considerations for addressing bladder, bowel, and sexual function needs of spinal cord injured armed forces.
- Uploaded on | 6 Views
-
 kavitha
kavitha
About Meeting the Needs of Spinal Cord Injured Armed Forces
PowerPoint presentation about 'Meeting the Needs of Spinal Cord Injured Armed Forces'. This presentation describes the topic on Sharon Wood, a Clinical Nurse Specialist in Neuro Urology and Sexual Health, discusses the important considerations for addressing bladder, bowel, and sexual function needs of spinal cord injured armed forces.. The key topics included in this slideshow are . Download this presentation absolutely free.
Presentation Transcript
1. Bladder, Bowel and Sexual Function Needs of our Spinal Cord Injured Armed Forces Sharon Wood Clinical Nurse Specialist Neuro-Urology and Sexual Function Royal National Orthopaedic Hospital
2. Why Neuro-Urology at an Orthopaedic Hospital The London Spinal Cord Injury Unit 12 acute beds 12 rehab beds 5 tissue viability beds 2 paediatric beds One of the 11 SCIC in the UK
3. General Population of SCI in UK UK population totals 58,789,194 (2001 Census) Est 40,000 SCI in UK (BASCIP 2001) Est 1200 new injuries each year In UK x 1 person paralysed every 8hrs, average age 32.6yrs Cost annually 500 million Not a reportable condition so data is incomplete BASCIP 2001 www.apparelyzed.com/statistics
4. Mortality following SCI 3179 pts (2 centres Stoke and Southport) 1943-1990 1 st Respiratory 2 nd Ischaemic heart disease 3 rd Injuries (including suicide) 4 th Urinary system (was 1 st pre 1972) 9 th Septicaemia Frankel et al (1998) Life expectancy tetraplegic post WW1 = 1 month Now 5yrs of normal life expectancy
5. General SCI Population Discharge 36.8% of patients leave a SCIC clinically depressed 21% of patients discharged from SCIC go to interim placements such as nursing homes or other institutions and not to their own property. Can take years to get an adapted property
6. Armed forces Majority of patients will be transferred to Queen Elizabeth Hospital in Birmingham Headley Court, Epsom Downs, Surrey 20 Neurology inpatient beds (inc brain injury and SCI) 46 beds polytrauma and medical conditions
7. Headley Court Recent refurbishment funded by Help for Heroes Charity
8. Demographics of Fatalities Iraq and Afghanistan Iraq 01/01/03 31/07/2009 Afghanistan 07/10/01 31/07/11 Total Killed 179 377 (379) Killed in Action 111 299 Died of Wounds 25 39 Other 43 39 Data from the UK Ministry of Defence Website (accessed 18/08/11)
9. Demographics of Injuries Iraq and Afghanistan Iraq 01/01/03 31/07/2009 Afghanistan 07/10/01 31/07/11 Casualites total 222 527 Very serious 73 259 Serious 149 269 Wounded in Action 315 1746 Non-battle Injury/disease 3283 3367 Aeromedical Evacuation 1971 4888 Data from the UK Ministry of Defence Website (accessed 18/08/11)
10. Published Papers USA 40 pts (513) = 9.8% Iraq only Head injury and Spinal Cord Injury Navy (Bethesda) and Army (Washington) Predominately blast injuries More than the Vietnam War Bell et al (2009) UK 25 pts (448) = 5% Iraq and Afghanistan Only cervical level Breeze et al (2011)
11. Armed forces discharges from service 2005-2010 Army Navy RAF Medically discharged 4539 1474 1049 Musculoskeletal cause 2777 (63%) 875 (62%) 429 (49%) Mental Behavioural 590 (13%) 176 (12%) 231 (26%) Data from the UK Ministry of Defence Website (accessed 18/08/11)
12. Pensions 141,715 war disablement pensioners (ongoing pension) 100% disablement rate = 327.72 per week
13. Referrals to RNOHT between 1994 Oct 2010 Total = 20 Navy = 1 Army = 9 Paratrooper = 2 RAF = 5 Marine = 1 Ex- SAS = 2 Rank Officer = 6 Non-officer = 14 2009/2010 referrals = 8 Referrals from Headley Court = 14 Referrals direct to SCIC for rehab = 6
14. Place of Main Rehabilitation 25% 40% 20% 20%
15. Where injured? Iraq 4 Afghanistan 6 (one at sea) UK - peacetime 7 Abroad - peacetime 3
16. Level and cause of injury Cervical 4 Fall (Disectomy) RTA Bullet Skiing Thoracic 7 Crush injury from vehicle x1 Fall x1 Diving x1 Helicopter crash x1 RTA x3 Lumbar 9 Epidural x1 IED x3 RTA x1 Bullet x1 Helicopter crash x1 Disectomy x1
17. Cause of injury Iraq and Afghanistan Iraq (4) Crush injury from jeep under fire = 1 RTA = 1 Bullet = 1 Helicopter crash = 1 Afghanistan (6) Fall (at sea) = 1 Bullet = 1 Fall from back of helicopter under fire = 1 Improvised explosive device = 3
18. Other morbidities Iraq and Afghanistan Head injury =1 Shoulder injury = 2 Fractured ankle = 1 Fractured ribs = 1 Dislocated hip = 1 Knee injury = 1 Limb amputations = 1 Blast/skin injuries = 1 Hand injury = 1 Internal abdominal bleeding = 1
19. Philosophy of Bladder and Bowel Management Patients Perspective Socially acceptable Simple Avoids drainage device Personal control Medical Perspective Low pressure storage Complete & efficient emptying Preservation of renal function Preservation of Renal Function Promotion of Continence Abrams et al (2008) A Proposed Guideline for the Urological Management of Patients with Spinal Cord Injury EAU (2011) Neurogenic Lower Urinary Tract Dysfunction NICE guidelines LUTS for men 2010 and urinary incontinence in women 2006 NICE due to publish Oct 2012 Incontinence in Neurological Disease Guidelines for the Management of the Neuropathic Bowel in Spinal Cord Injury (2009)
20. Bladder Management
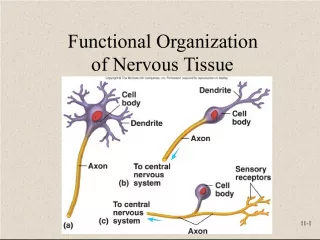
21. Upper Motor Neurone SCI (T12 and above) CC X SMC PMC X Loss of inhibitory impulses cause neurogenic detrusor overactivity Urethra and sphincters also overactive & unco-ordinated Detrusor sphincter dyssynergia (DSD) High pressure voiding which may cause kidney damage Incontinence due to uncontrolled emptying Loss of bladder sensation and voluntary control
22. External Sphincter dysnergia Trabeculation Diverticulum Detrusor Pressure Urine Flow Neurogenic detrusor overactivity Intraurethral Pressure Sphincter EMG Sphincter Dyssynergia Neurogenic Detrusor Overactivity Fir tree
23. Neurogenic Detrusor Overactivity Detrusor Sphincter Dyssynergia INFECTION Renal Failure REFLUX What happens if we dont treat it?
24. Lower Motor Neurone SCI (L1 and below) Under-active detrusor acontractile detrusor Under-active sphincter and urethra sphincter incompetence No sensation of bladder fullness Flaccid bladder, no spontaneous voiding or voluntary control CC X SMC X PMC X X X X
25. Diagnosis of Bladder Dysfunction Cervical- 4 Thoracic- 7 Lumbar- 9 NDO 3 4 0 NDO + DSD 0 2 1 Acontractile 0 1 2 Acontractile + USI 0 0 5 Unknown 1 (not RNOHT) 0 1 (not RNOHT)
26. Type of Bladder Management Cervical patients all on anticholinergics Thoracic patients 4 pts on anticholinergics, 1 pt acontractile, 1 pt old SARSI Lumbar patients 1 pt on anticholinergics
27. Penis Holder Grips
28. Bowel Management
30. Neurogenic Bowel Upper motor neurone T12 and above Reflex bowel Tight anal sphincter Lower motor neurone L1 and below Flaccid bowel Weak anal sphincter
31. Bowel Management Reflex T12 and above Balanced high fibre diet 2000ml fluid per day Suppositories, DRE and Manual evacuations (DRF) Gastro colic reflex Abdominal massage Positioning Regular exercise Flaccid L1 and below Balanced high fibre diet 2000ml fluid per day Abdominal massage/ straining Gastro colic reflex Manual evacuations Positioning. Regular exercise Aperients
32. Bowel Management according to level of injury Cervical Thoracic Lumbar DS + ME 2 3 Anal Irrigation (Peristeen) 1 2 2 Spontaneous evacuation 1 1 3 Colostomy 0 0 1 Unknown 0 1 3 Medication = Movicol, Docusate Sodium and Senna Ano-physiology tests done in 3 patients
33. So what is the Stanmore hand shake? It is a necessary procedure called a Digital Stimulation and then Manual Evacuation
34. Trans anal irrigation 25% of patients
35. Bladder and Bowel management has to fit into their life not lead it
36. Sexual Function and Disability EAU (2010) Sexual Dysfunction: Erectile Dysfunction and Premature Ejaculation Update on guidelines in sexual dysfunction assessment, treatment and management
37. Male SCI Upper motor neurone Reflex erections in 95% Ejaculation possible in 5% complete and 32% incomplete Lower motor neurone 25% able to have some type of erection Ejaculation possible in 18% complete and 70% in complete (Fazio and Brock 2004) Cauda equina injuries No erectile activity
38. Cervical Level Injury Erectile and Fertility Function Total pts = 4
39. Thoracic Level Injury Erectile and Fertility Function Total pts = 7
40. Lumbar Injury Erectile and Fertility Function Total pts = 9
41. Incidence of SD General Population Men 1 in 10 adult males experience sexual dysfunction Important that my patients know that it isnt always a disabled persons problem
42. Fertility post SCI Semen quality reduces at approx 2 weeks post injury Abnormal sperm motility and viability not sperm count Related to at least one abnormal hormonal level (51%) and hypothalamic-pituitary axis abnormality (86%) Better bladder management and less infections help. Repeated ejaculation with Ferticare vibrator or electroejaculation can improve semen quality Ultimately, best to take samples for fertility treatment from testicular biopsies Patki et al (2008)
43. Marriage and relationships Delvio and Richards 1996 Marriage more sustainable if higher education If divorced pre/peri injury then more likely to have a successful post injury marriage Women less likely to marry than men and divorce and separation is higher in women with SCI Lack of social exposure/accessible buildings, social skills, pre- existing personality/behavioural difficulties Pearcy et al 2007 Relationships are more likely to fail in acute rather than rehab stage Disempowerment, over assistance, family and friends are motivators though Information/education of activities
44. SCI perceptions of themselves sexually Anderson et al 2007 Direct link between sexual function and quality of life. 87.9% sexually active post SCI increased with age of injury 83.2% altered sense of themselves as a sexual person Intimacy, sexual need, self-esteem, to keep a partner Fear of bladder and bowel accidents Autonomic dysreflexia directly related to bladder/bowel management and sensitivity. Can be sexually stimulating
45. Body image of all the symptoms associated with physical disability, the most oppressive and destructive is the radical loss of self-esteem Barbin and Ninot 2008 Skiing increased perception of an attractive body. Athletic identity, increased confidence BACKUP
46. Important message You can still have an active sex life You can still have children if you want to You still have the same modes of arousal Brain,Tactile and Orgasm It may not be exactly the same as before but can be just as good
47. Neuropathic Pain 60%
48. Psychology 40% 20%
49. Change in patients status From independent to dependent directing own care Partners should not be carers Financial pressures Compensation claims can go on for years Ego Patient not a sexual person Rehabilitation encourages empowerment, independence and re-integration back into society
50. Outcomes Coping strategies (social reliance) has a direct impact on functional and rehabilitation outcomes Kennedy et al (2011) Functional outcome better and length of stay shorter if rehab is in a specialist SCIC New et al (2011)