Methods and Considerations for Glucose Measurement in Clinical Chemistry

This article discusses various methods for measuring glucose levels in clinical chemistry, including considerations for laboratory testing and glucose preservation. It also covers reference values for different types of specimens and collection methods.
- Uploaded on | 0 Views
-
 loganblanda
loganblanda
About Methods and Considerations for Glucose Measurement in Clinical Chemistry
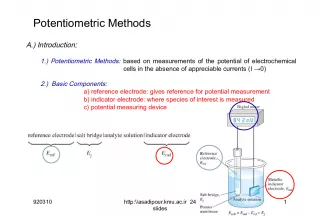
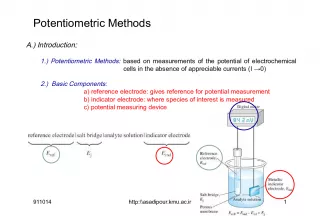
PowerPoint presentation about 'Methods and Considerations for Glucose Measurement in Clinical Chemistry'. This presentation describes the topic on This article discusses various methods for measuring glucose levels in clinical chemistry, including considerations for laboratory testing and glucose preservation. It also covers reference values for different types of specimens and collection methods.. The key topics included in this slideshow are MLAB 2401, clinical chemistry, glucose measurement, diabetic management, laboratory testing,. Download this presentation absolutely free.
Presentation Transcript
1. MLAB 2401: Clinical Chemistry Keri Brophy-Martinez MLAB 2401: Clinical Chemistry Keri Brophy-Martinez Methods of Glucose Measurement and Diabetic Management
2. Laboratory testing Laboratory testing Considerations Reference values depend on: Type of specimen venous/capillary Serum, plasma, whole blood How was it collected? fasting, random, after a meal Reference value (serum/plasma) 74-106 mg/dL 2
3. Laboratory testing Laboratory testing Glucose preservation Perform testing < 1 hour after collection Separate plasma from cells < 1 hour Cells continue to utilize glucose at a rate of 10 mg/dL per hour. Refrigeration slows the process. Collect blood in sodium fluoride tube Grey top tube Fluoride inhibits glycolysis 3
4. Specimen Collection Specimen Collection Whole blood Point of care Results are @ 11% lower than plasma/serum Serum Plasma 4
5. Other Specimen Types Other Specimen Types CSF specimens Analyzed ASAP Glucose level is 60-70% of pts current blood level. CSF glucose in Fasting (non-diabetic) @ 40-70 mg/dL Decreased CSF glucose values suggest bacterial meningitis because bacteria are consuming glucose as an energy source Normal or Increased CSF glucose suggests viral meningitis. 24 hour urine A small amount of glucose is lost in the urine daily. Usually < 500mg/24 hr. Random urine for diagnosis no longer performed, but some patients use it for self monitoring. 5
6. Methods for Glucose Determination Methods for Glucose Determination
7. Glucose Oxidase Methodology Glucose Oxidase Methodology 7 Glucose + O 2 + H 2 O Glucose Oxidase Gluconic acid + H 2 O 2 H 2 O 2 + Chromogen Oxidized chromogen + H 2 O Peroxidase Trindler reaction Glucose oxidase an enzyme that will catalyze the reaction of glucose to gluconic acid, with the formation of hydrogen peroxide as a by-product
8. Glucose oxidase Glucose oxidase Good methodology, but: Procedure is good for blood and CSF specimens, but urine has too many interfering substances. Subject to interference from ascorbic acid, bilirubin and uric acid which are also oxidized by peroxidase. Alternative way to determine concentration: (polarographically) Measuring the amount of oxygen used up by an electrode 8
9. Hexokinase Hexokinase An enzyme that catalyzes the phosphorylation of glucose Method can be very accurate and precise since the coupling reaction is specific Time consuming for routine use Reference methodology since it lacks interferences associated with glucose oxidase method Procedure can utilize blood, urine and CSF 9
10. Hexokinase Methodology Hexokinase Methodology 10 Glucose + ATP Hexokinase Glucose 6 Phosphate + ADP Glucose 6 - Phosphate + NADP G6PD NADPH + H + 6-Phosphogluconate NADP - Nicotinamide adenine dinucleotide phosphate (oxidized form) is reduced NADPH - reduced form absorbs light (340nm) proportional to the amount of glucose present in first reaction
11. Laboratory Diagnosis Laboratory Diagnosis
12. Laboratory Tests Laboratory Tests Fasting blood sugar (FBS) Most frequently ordered screening test for glucose metabolism Reference value: 74-106 mg/dL Fasting values > 126 mg/dL usually indicate a problem FBS should be repeated on another day to confirm diagnosis Borderline diabetes may have a normal FBS & may need a challenge test to demonstrate abnormality 12
13. 2 hr post prandial Laboratory Tests 2 hr post prandial Laboratory Tests 2 Hour Postprandial Patient has FBS drawn Ingests a 75 gram high carbo breakfast or sometimes drinks glucola Has repeated glucose test at 2 hours Glucose level should have returned to fasting levels. If glucose > 200 mg/dL on the postprandial test, a fasting or random glucose level, should be performed on a subsequent day to diagnose with diabetes 13
14. Laboratory Tests Oral glucose tolerance test (GTT) No longer recommended by the new ADA guidelines Used to screen for gestational diabetes Problems included calculation dosage, patient must drink it, keep it down, stay relatively inactive during test period, and be successfully drawn on time. 14
15. Oral glucose tolerance test (GTT) Oral glucose tolerance test (GTT) Patient directions - important. Eat an adequate carbohydrate diet at least three (3) days prior to test Evening before the test, no eating after supper meal Test is begun in early a.m. Obtain fasting specimen Test dose: ** test dose has been reduced to 75 gm for adults and 1.75 gm / kg for children. Test dose must be consumed within 5 minutes. Patient is to remain resting, no smoking or eating during test period Blood and urine specimens are collected at hourly intervals - Testing of the urine glucose & ketones, no longer routine. 15
16. Oral glucose tolerance test (GTT) Normal Abnormal
17. Laboratory Tests: Ketones Laboratory Tests: Ketones Produced by the liver Metabolism by-products of fatty acids Three bodies Acetone (2%) Acetoacetic acid (20%) 3- hydroxybutyric acid (78%) Increase in cases of carbohydrate deprivation or decreased carbohydrate use (diabetes mellitus, starvation/fasting, prolonged vomiting etc.)
18. Laboratory Tests: Microalbumin Laboratory Tests: Microalbumin Microalbumin Persistent albuminuria in the range of 30-299 mg/ 24 h or an albumin-creatinine ratio of 30-300 g/mg Indication of renal nephropathy Assists in the diagnosis of early proteinuria Normal urine dipsticks are insensitive to low concentrations of urine albumin
19. Glycosylated Hemoglobin/ Hemoglobin A1c Glycosylated Hemoglobin/ Hemoglobin A1c Long term glycemic control indicator, reflects average blood glucose level over the previous 2-3 months Glucose molecule attaches nonenzymatically to the hemoglobin molecule Advantages: Time average glucose not subject to temporary variability due to diet and exercise Does not require fasting Influenced by: Conditions that affect the life span of the RBC, such as sickle cell disease and hemolytic diseases Hemoglobin A 1C is the most commonly measured glycosylated hemoglobin 19
20. Glycosylated Hemoglobin/ Hemoglobin A1c Glycosylated Hemoglobin/ Hemoglobin A1c Specimen : EDTA whole blood doesnt need to be fasting Measured by electrophoresis, enzymatic assays, HPLC Hemoglobin A 1C reference range 4.0 - 6.0 % For diagnosis of diabetes based on Hemoglobin A 1C results, the patient must has a result of > 6.5% , confirmed by repeat measurement.
21. Other related tests: Lactose Tolerance Other related tests: Lactose Tolerance Lactose - disaccharide Lactose malabsorption or lack of enzyme needed to breakdown lactose Often results in diarrhea, cramping, and gas Lab evaluation Perform OGTT using lactose, not glucose Normal GTT curve similar to OGTT (glucose level will increase 25 mg/dL above the fasting level). Lactase deficiency Flat curve - no/very little increase in glucose level. 21
22. Urine Glucose Urine Glucose Copper Reduction- Clinitest Not specific Detects all reducing sugars Used to detect galactosemia in babies and children < 3 yrs old.
23. References References Bishop, M., Fody, E., & Schoeff, l. (2010). Clinical Chemistry: Techniques, principles, Correlations. Baltimore: Wolters Kluwer Lippincott Williams & Wilkins. Sunheimer, R., & Graves, L. (2010). Clinical Laboratory Chemistry. Upper Saddle River: Pearson . 23