Overview of Ontario Health System Funding Reform

Irene Blais, Director of the Funding Unit, presents an overview of the Ontario Health System Funding Reform and the role of CCOs. The presentation covers current QBPs, systemic treatment, GI endoscopy, new QBPs, cancer surgery, colposcopy, and Q&A.
- Uploaded on | 3 Views
-
 aliana
aliana
About Overview of Ontario Health System Funding Reform
PowerPoint presentation about 'Overview of Ontario Health System Funding Reform'. This presentation describes the topic on Irene Blais, Director of the Funding Unit, presents an overview of the Ontario Health System Funding Reform and the role of CCOs. The presentation covers current QBPs, systemic treatment, GI endoscopy, new QBPs, cancer surgery, colposcopy, and Q&A.. The key topics included in this slideshow are Ontario Health System, funding reform, CCOs, QBPs, cancer surgery,. Download this presentation absolutely free.
Presentation Transcript
1. Ontario Health System Funding Reform: Overview Presentation by: Irene Blais, Director, Funding Unit Date: Wednesday September 11 th , 2013 CAPCA Chief Operating Officer Roundtable
2. Agenda Health System Funding Reform and CCOs Role Current QBPs Systemic Treatment GI Endoscopy New QBPs Cancer Surgery Colposcopy Q & A 2
3. Health System Funding Reform and CCOs Role 3
4. Health Service Providers (e.g. Community Care Access Centres, Hospitals) Global Funding HSFR What is Health System Funding Reform Vision? 4 Evidence-based funding driven based on the highest quality, most efficient care How many patients they look after The services they deliver The evidence-based quality of these services The specific needs of the population they serve Slide provided by MOHLTC
5. Funding Reform: Two Key Components 5 1. Health Based Allocation Model (HBAM) HBAM is a made-in-Ontario model that informs funding allocation to health services providers based on population needs 2. Quality-Based Procedures (QBP) Price x volume, evidence based clinical pathways ensure quality standards Opportunity for process improvements, clinical re-design, improved patient outcomes, enhanced patient experience
6. Patient-Based Funding will include HBAM and Quality- Based Procedures Patient-Based Funding is based on clinical activities that reflect an individuals disease, diagnosis, treatment and acuity Hospitals, Community Care Access Centres and Long Term Care are the first sectors incorporated into the funding strategy Health System Funding Reform Patient-Based Funding (70%) Health Based Allocation Model (40%) Quality-Based Procedures (30%) Global (30%) HSFR: The model 6
7. Recap : An evidence and quality-based framework has identified Quality-Based Procedures that have the potential to both improve quality outcomes and reduce costs 7
8. 2013/14 Funding Allocation Update 8 Slide provided by MOHLTC
9. CCO/ORN leading full implementation of Quality-Based Procedures including Quality-Based Procedures Definitions Best Practices Better Practice Hospitals Clinical Handbooks Clinical Engagement Clinical Quality-Based Procedure Best Practice Price Quality Overlay Framework Pricing/ Funding Capacity Planning Integrated Quality-Based Procedure Scorecard Monitoring and Evaluation Regional/System Volume Management/Capacity Planning Strategy Capacity Utilization and Forecasting Program 9 Products Product Details
10. Why is CCO part of HSFR? Governments Advisor for Cancer & Renal Services. Principles of equity, evidence-based recommendations, performance-oriented goals, and value for money (help build the best health system in the world) Motivate change through the cause, evidence and data, and funding levers Oversee more than $800 million in patient-based funding Robust clinical leadership model based on regional networks Well-developed evidence review and guideline development processes Well-developed performance management model 10
11. Current QBPs Systemic Treatment 11
12. Why Reform Systemic Therapy? Limitations of the Current Model 12 Consult Treatment start Further treatment RCC Patient does NOT require treatment $3400 Funding Provided RCC RCC RCC $3400 RCC RCC RCC $3400 + $3300 RCC RCC Community Hospital Systemic Treatment if funded in a variety of ways: RCCs: Lifetime payment triggered by a consultation (C1S) Non-RCCs: Per case (unique patient) or funding per visit in some cases Some facilities receive PCOP funding (per visit) This results in: Inequities: Not all hospitals receive funding for systemic treatment Duplication: In some cases, double-payment exists
13. How will the new funding model address these limitations? Move from a lifetime payment approach to an activity-based bundled payment approach A Bundled payment approach allows funding to follow the patient, thereby: Recognizing incident and prevalent cases Particularly important as survivorship improves Reducing & eventually eliminating inequities in funding Supporting the shared care model (resulting from a consistent/fair funding model) Recognizing the work associated with the delivery of oral chemotherapy regimens Incent for high-quality care: Identifying and funding for appropriate care according to evidence-informed practice Ensuring patients get access to care they need Optimizing use of resources 13 Developing a new funding model for systemic treatment is a priority for CCO under the RSTP Provincial Plan released in 2009
14. Move from a lifetime payment approach to funding for specific bundles of activity to funding that follows the patient The Bundled Payment Model- Phased Approach 14 Parenteral Treatment- Adjuvant, Curative, Neo-Adjuvant Developed & undergoing validation, 2014-15 implementation Parenteral Treatment- Adjuvant, Curative, Neo-Adjuvant Developed & undergoing validation, 2014-15 implementation Other treatment bundles: - Parenteral Treatment-Palliative - Oral Treatment (may be multiple bundles) To be developed for 2014-15 implementation Other treatment bundles: - Parenteral Treatment-Palliative - Oral Treatment (may be multiple bundles) To be developed for 2014-15 implementation Consultation Treatment/ Follow-up Follow-up ( may be multiple bundles) To be developed for 2014-15 implementation Follow-up ( may be multiple bundles) To be developed for 2014-15 implementation Consultation for Systemic Treatment Developed and to be implemented 2014/15 Diagnosis/ Staging Bundle For future phase development & implementation
15. 15 DSG Chair Review - Identify standard regimens and evidence- informed practice for each regimen -Feedback incorporated (follow-up call if reqd) & sent back to DSG Chairs for validation All DSG Member Review -All DSG members review list of standard regimens for their Disease Site -DSG members to provide feedback re: evidence-informed regimens DSG Chair Follow-up Calls - Follow-up calls with DSG Chairs (if required) to incorporate feedback from All DSG Member Review All Practitioner Review -All Disease site regimens sent to all practitioners for feedback re: evidence-informed regimens Validating Evidence- Informed Practice Next Steps: 1. Incorporate feedback from all DSG Member Review(where appropriate) 2. All Practitioner Review (fall 2013)
16. Current QBPs GI Endoscopy 16
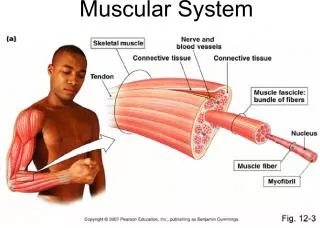
17. Scope of GI Endoscopy QBP 17 GI Endoscopy Activity in Hospitals ( 517,788 cases in 2011/12) Colonoscopy Inspection procedures Gastroscopy Inspection procedures Excision/Biopsy/Destruction procedures Other GI Endoscopy: ex. EUS, ERCP and Laser procedures Hospital Care Setting Endoscopy suite Day Surgery Room Inpatient Emergency Room Expenses $139M in hospital direct costs (2011/12) Pathology laboratory is out-of-scope Physician fees are out-of-scope
18. Scope of GI Endoscopy QBP Evidence gathered during QBP development suggests that the colonoscopy QBP should be expanded to include all endoscopy services: 1. Better patient care when multiple interventions are required 2. Many services performed in the endoscopy suite, and the associated resources, cannot be decoupled 3. The quality agenda for colonoscopy and endoscopy are tightly aligned 4. Economies of scale exist when multiple endoscopy services are preformed together 5. Overlap of funding across the breadth of services provided in an endoscopy suite is substantial 18
19. Scope of GI Endoscopy QBP 19 The table above summarizes the number of G.I Endoscopy procedures by procedure combination in each of the 4 identified settings in 2011/12. The 11 procedure combinations are mutually exclusive meaning that a patient encounter can only be mapped to one combination. The total expenses for these procedures are estimated at $139MM based on 2011/12 data
20. New QBPs Cancer Surgery 20
21. Cancer Surgery Agreements (CSA) to Quality Based Funding (QBP) CCO has been advising the Ministry of Health and Long-Term Care on the allocation of incremental funding for cancer surgery procedures since 2004 Good progress decrease in wait times Strong linkage to quality via Schedule B Cancer Surgery is well positioned for transition to QBP Strong quality program & guidelines & pathways Benefit from knowledge gained from CSA process & methodology Disease site approach Prostate will be the initial disease site Unknown possible that CSA will exist for some disease sites
22. Annual Cancer Surgery Volumes 2004/05 2012/13 (incremental funding $70MM 2012/13) 22 Fiscal Year Total Volume All Incremental Funded Incremental Unfunded Volume 2004/05 27,569 1,145 1,145 0 2005/06 37,441 3,300 3,300 0 2006/07 44,696 4,329 4,329 0 2007/08 43,610 5,237 5,041 (196) 2008/09 46,384 7,008 5,379 (1,629) 2009/10 41,904 7,828 6,414 (1,414) 2010/11 47,265 6,438 6,438 0 2011/12 41,802 8,166 8,166 0 2012/13 43,691 8,497 7,968 (529)
23. Cancer Surgery Wait times 23
24. New QBPs Colposcopy 24
25. Current State - Colposcopy In Ontario, colposcopies are conducted both in hospitals and also within the community, primarily private practitioner offices and clinics. Based on clinical expert feedback at CCO, variations in practice exist in all settings across the province of Ontario. In addition, a consistent, system-wide approach for accountability over the quality and efficacy of colposcopy services provided does not exist. The 2008 Program In Evidence-Based Care (PEBC) Colposcopy standards (which describe the optimum organization for the delivery of colposcopy services in Ontario) are currently in the process of being revised. 25
26. Current State - Colposcopy CCO foresees the need to include both hospitals and community settings in order to appropriately apply these standards across the province of Ontario. Practice variations, as well as the lack of consistent mechanisms for measuring quality, each present an opportunity to increase quality and efficiency across the system by including both hospitals and community settings in the definition of the Colposcopy QBP. The Colposcopy QBP aims to improve quality, decrease wait times and reduce lost-to-follow-up rates. 26
27. Current State - Colposcopy 27 Colposcopy Summary FY 2011/12 (Source: OHIP) Count of procedures by Location and Ohip Fee Code #S744 Z729 Z730 Z731 #Z766 Z787 Total Total Hospital 3,613 1,971 32,047 28,219 3,874 9,507 79,231 56% Non-Hospital* 772 1,050 27,129 25,593 1,699 5,036 61,279 44% Total 4,385 3,021 59,176 53,812 5,573 14,543 140,510 100% 3% 2% 42% 38% 4% 10% 100% * OHIP records where the hospital master number was blank and it was assumed that the procedure happened in a non- hospital setting OHIP Code Description #S744 Cervix- cone biopsy - any technique with or without D&C Z729 Cryoconization, eletroconization or CO2 laser theraphy with or without curettage for premalignant lesion (dysplasia or carcinoma insitu), outpatient procedure Z730 Follow-up colposcopy without biopsy with or without endocervical curetting Z731 Initial investigation of abnormal cytology of vulva and/or vagina or cervix under colposcopic technique with or without biopsy(ies) and/or endocervical curetting #Z766 Loop Electrosurgival Excision Procedure (LEEP) Z787 Follow-up colposcopy with biopsy(ies) with or without endocervical curetting
28. Next Steps Policy and Strategy Continued Policy and Strategy development including but not limited to: Cancer funding Think Tank Funding across multiple sectors including homecare Models of Care Environmental scan Evaluation framework 28
29. 29