Upper Cervical Trauma: The Anatomy, X-rays, and Fractures

This article discusses upper cervical trauma, also known as cranio-cervical trauma, occipito-cervical trauma, or occipito-atlanto-axial trauma. It covers the anatomy of the upper cervical spine, X-rays, and fractures of the O, C1, and C2 vertebrae.
- Uploaded on | 6 Views
-
 klara39
klara39
About Upper Cervical Trauma: The Anatomy, X-rays, and Fractures
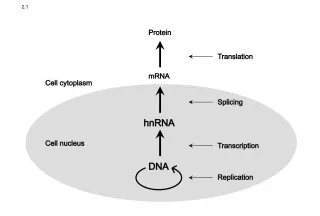
PowerPoint presentation about 'Upper Cervical Trauma: The Anatomy, X-rays, and Fractures'. This presentation describes the topic on This article discusses upper cervical trauma, also known as cranio-cervical trauma, occipito-cervical trauma, or occipito-atlanto-axial trauma. It covers the anatomy of the upper cervical spine, X-rays, and fractures of the O, C1, and C2 vertebrae.. The key topics included in this slideshow are Upper cervical trauma, cranio-cervical trauma, occipito-cervical trauma, occipito-atlanto-axial trauma, anatomy, X-rays, fractures,. Download this presentation absolutely free.
Presentation Transcript
1. Upper Cervical Trauma Upper Cervical Trauma Sohail Bajammal, MBChB, MSc Sohail Bajammal, MBChB, MSc November 14, 2006 St. Josephs Healthcare, Hamilton Weekly Orthopaedic Teaching Rounds
2. Upper Cervical Trauma Upper Cervical Trauma a.k.a. Cranio-cervical Trauma Occipito-cervical Trauma Occipito-atlanto-axial Trauma
3. Outline Outline The Problem Anatomy X-rays Fractures of O, C1, C2
4. The Problem The Problem Better recognition Better pre-hospital care (ATLS, Orthopod) Radiographic finding Improved cars safety: Less mortality at scene, more of OC injury
5. Evaluation Evaluation History: mechanism of injury Physical: ATLS 2 survey: thorough neurological exam Radiology: 3-views C-spine, CT, MRI
6. Anatomy Anatomy
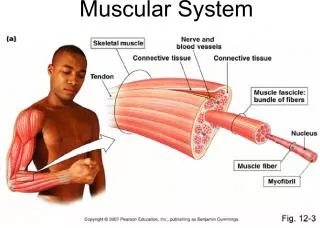
7. Anatomy Anatomy Unique anatomy of O-C1-C2 C1: no body, 2 articular pillars connected by 2 arches C2: dens, flat C1-2 Ligaments: Intrinsic (within spinal canal): Odontoid: alar, apical Cruciate: transverse lig, vertical bands Tectorial membrane: thickening of PLL Extrinsic: Ligamentum nuchae Anterior and posterior atlanto-occipital membrane Anterior and posterior atlanto-axial membrane Joint capsules Vertebral artery
8. Courtesy of AnatomyTV
15. Ponticulus Posticus Latin , little posterior bridge Ponticulus Posticus Latin , little posterior bridge Young et al., 2005 JBJS(A) 15.5% prevalence of arcuate foramen in 464 lateral c-spine x-rays
16. Ponticulus Posticus Ponticulus Posticus
17. Ponticulus Posticus Ponticulus Posticus
18. X-rays X-rays
19. Cervical X-rays ABCDEs Cervical X-rays ABCDEs A: adequacy, alignment B: bones C: cartilage D: disc space E: else (skull, clavicle) S: soft tissue
20. Lateral C-spine Lateral C-spine
21. Harris Lines Harris Lines SAC: > 13 mm
22. BC/OA >1 considered abnormal Limited Usefulness Positive only in Anterior Translational injuries False Negative with pure distraction Powers Ratio
23. Open-mouth View Open-mouth View
24. Occipital Condyle Fractures Occipital Condyle Fractures CT, R/O OC dissociation I: comminuted, axial impaction Stable Collar 6-8 weeks II: extension of basilar skull fracture into condyle Potentially unstable Collar 6-8 weeks III: avulsion of alar lig Minimal displaced Halo vest, 8-12 weeks Displaced O-C2 fusion Consider surgery if OC dissociation
25. Occipito-cervical Dissociation Occipito-cervical Dissociation Rare and usually fatal Often assoc. with facial injuries, chest trauma Deceleration AVOID traction!! Halo until surgery 1 treatment: Oc-C2 fusion if good screw purchase Oc-C3 fusion otherwise Biomechanically: plate & screw > screws > wires
26. Traynelis Classification of Occipito-cervical Dissociation Traynelis Classification of Occipito-cervical Dissociation
27. Harborview Classification of Occipitocervical Injury Harborview Classification of Occipitocervical Injury I: MRI: hemorrhage or edema at OC junction Normal Harris lines No distraction on traction test with 25 lb of traction II: MRI: hemorrhage or edema at OC junction Normal Harris lines < 25 lb traction: sufficient distraction to meet OC dissociation thresholds of Harris III: Static imaging: distraction beyond thresholds of Harris
28. Atlas (C1) Fractures Atlas (C1) Fractures 10% of all cervical fractures Rare neurological deficits; if any, R/O dissociation 50% concomitant fractures Morphological classification 1. Posterior arch: hyperextension 2. Lateral mass: rotation or lateral flexion forces 3. Anterior arch fractures (blowout or plow fractures) : hyperextension, 4. Bursting-type fractures (Jefferson): symmetrical axial load 5. Transverse process 6. Anterior tubercle
29. Atlas Fractures Atlas Fractures The extent of lateral mass separation is more relevant than the number of fracture fragments
30. Stable Atlas Fractures Stable Atlas Fractures Posterior arch fracture: collar 10-12 weeks Anterior arch avulsion fracture: collar C1 ring fracture with <7 mm of overall lateral mass displacement: collar or halo
31. Unstable Atlas Fractures Unstable Atlas Fractures C1 ring fracture with 7 mm of overall C1 lateral mass displacement: prolonged halo or fusion (C1-C2, or Occiput-C2) Plough fracture: reduction with halo in slight flexion or C1-C2 fusion or occiput-C2
32. Plough Fracture Plough Fracture
33. Rupture of Transverse Ligament Rupture of Transverse Ligament Flexion force Dickman Classification: I. Mid-substance tear II. Avulsion of lateral mass of C1 As force increases, alar and apical lig tear (ADI > 7mm) Treatment: If ADI 5mm collar If ADI >5mm and type I C1-C2 fusion If ADI >5mm and type II halo
34. Atlanto-Axial Instability Atlanto-Axial Instability A: Rotational Around the dens Treated with closed reduction and immobilization. Beware of associated fractures B: Translational Translation between C1C2, where transverse lig is disrupted Mid-substance transverse ligament tears (type I) are treated with C1C2 arthrodesis C: Distraction: Indicating craniocervical dissociation Bony avulsions (type II) may be treated with halo or C1C2 arthrodesis
35. Rotatory Atlanto-Axial Instability Rotatory Atlanto-Axial Instability Collar or Halo C1-C2 Fusion
36. Axis (C2) Fractures Axis (C2) Fractures Odontoid fractures Traumatic spondylolisthesis of the axis (hangman's fracture)
37. Odontoid Fractures Odontoid Fractures 60% of C2 fractures 10-20% of all c-spine fractures Neurological deficits in 10-20% Bimodal: young (high energy), elderly (falls) Anderson and D'Alonzo Classification
39. Type I Odontoid Type I Odontoid Occurs at tip, cephalad to the transverse Least common Represent an avulsion of the alar ligament Treated with collar or halo 6-8 weeks Surgery (occiput-C2 fusion) if associated with occipitocervical dissociation
40. Type III Odontoid Type III Odontoid Extends into the body of the axis More stable than type II fractures Higher union rate with non-surgical Treated with a halo or brace 8-12 weeks after reduction if displaced
41. Type II Odontoid Type II Odontoid At the junction of the base of the odontoid and body of the axis The most common fracture type The least likely to heal with non-surgical (10-77% non-union) IIA: new addition, comminution at base Treatment: controversial
42. Type II Odontoid Type II Odontoid Higher risk of non-union: Initial displacement > 5mm Posterior displacement Angulation > 10 0 Age > 50 Smoking Delay in diagnosis > 3 weeks Inability to achieve or maintain reduction
43. Options for High Risk type II Options for High Risk type II 1. Collar: very high risk of non-union 2. Reduction and Halo: risk of complications in elderly 3. Anterior Odontoid Screw(s) Pros: High union rate, preserves atlanto-axial motion Cons: Poor fixation in osteoporotic, difficult in large chest or posteriorly displaced C/I: reverse obliquity 4. Posterior C1-C2 arthrodesis: C1-2 transarticular screw > segmental C1-2 fixation > wires techniques
44. Anterior Odontoid Screw Anterior Odontoid Screw
45. Traumatic spondylolisthesis of the Axis (Hangman's fracture) Traumatic spondylolisthesis of the Axis (Hangman's fracture) 2 nd most common fracture of C2 15% of all cervical spine fractures Higher energy injury, associated spinal #: 30% Younger age group, MVC MOI: hyperextension + axial compression; additional flexion moment leads to very unstable injury Rare neurological involvement
46. Hangman's Fracture Effendi Levine & Edwards Classification Hangman's Fracture Effendi Levine & Edwards Classification
47. Type I Hangmans Type I Hangmans Most common Bilateral pars fractures with translation <3 mm and no angulation Treated with collar, occasionally halo
48. Type IA Hangmans Type IA Hangmans Atypical fracture, recently recognized Minimal translation and little or no angulation Elongation of the C2 body CT: extension of fracture line into the body and often through the foramen transversarium (vertebral artery injury may occur) May have canal compromise Usually halo, surgery if neuro deficits Surgical options: anterior C2C3 arthrodesis, posterior C1C3 vs C2C3 arthrodesis, or combined approach
49. Type IA Hangmans Type IA Hangmans
50. Type II Hangmans Type II Hangmans C2-3 disc and PLL are disrupted, resulting in translation >3 mm and marked angulation ALL generally remains intact but is stripped from its bony attachment Halo: after reduction in slight extension
51. Type IIA Hangmans Type IIA Hangmans Less common; MOI: hyperext, axial then flex Fracture line is more oblique than vertical (vs II) Little or no translation, but significant angulation. Avoid traction Halo, and if markedly displaced, possibly direct fixation of fractured arch through a posterior approach C1-C3, or by C2C3 anterior discectomy and arthrodesis
52. Type III Hangmans Type III Hangmans A combination of pars fracture with dislocation of the C2-3 facet joints Very unstable, with free-floating inferior articular processes The most common injury to be associated with neurological deficit Requires surgery; it is irreducible by closed means Options: Anterior C2-3 discectomy and fusion, or posterior open reduction and C1-3 fusion
53. Posterior C1-2 Fusion Gallie Technique Posterior C1-2 Fusion Gallie Technique
54. Posterior C1-2 Fusion Brooks-Jenkins technique Posterior C1-2 Fusion Brooks-Jenkins technique
55. C1C2 Transarticular Screw Fixation Magerl technique C1C2 Transarticular Screw Fixation Magerl technique
56. Finally.. Its over! Finally.. Its over!
57. Halo Halo Crown first then the vest Prep areas in infiltrate with local Normally put scoop under head (unless contraindicated) Put halo crown around head Landmarks: for the anterolateral pins, 1cm above the lateral 1/3 of the eyebrow and the same distance above the top of the ear Place the anterior pins in bare skin NOT in the hairline
58. Halo Halo Have patient close eyes before insertion of ant pins Place 4 pins in and tighten all 4 to engage skin and bone Tighten to 8 in-lb with the torque wrench Place the vest on X-ray!
59. Halo Care Halo Care Routinely retighten after 24-48 hours If a pin is to be replaced, a new pin should be inserted satisfactorily before the loose pin is removed Pin sites should be cleaned daily Most commonly injured nerves are the supraorbital and supratrochlear
60. Halo Care Halo Care Inserting anterolateral pins behind the hairline in hopes of obtaining a more cosmetically acceptable scar should be avoided - this location places the pin within the temporal fossa where the skull is the thinnest Pins located in the temporal fossa also pierce the temporalis muscle and often lead to painful mastication