Coronary Artery Disease: Epidemiology, Risk Factors, and Prevention

Atherosclerosis is the leading cause of death and disability worldwide, with clinical manifestations like angina, MI, sudden death, TIA, stroke, claudication, gangrene, and hypertension. Learn about the risk factors, pathogenesis, and prevention options of coronary artery disease from a staff cardiologist.
- Uploaded on | 2 Views
-
 yanaika
yanaika
About Coronary Artery Disease: Epidemiology, Risk Factors, and Prevention
PowerPoint presentation about 'Coronary Artery Disease: Epidemiology, Risk Factors, and Prevention'. This presentation describes the topic on Atherosclerosis is the leading cause of death and disability worldwide, with clinical manifestations like angina, MI, sudden death, TIA, stroke, claudication, gangrene, and hypertension. Learn about the risk factors, pathogenesis, and prevention options of coronary artery disease from a staff cardiologist.. The key topics included in this slideshow are . Download this presentation absolutely free.
Presentation Transcript
1. C oronary Artery Disease Punit Goel, MD Asst Professor in Cardiology, University of Missouri Hospital & Clinics Staff Cardiologist, Harry Truman VA Hospital
2. Epidemiology Risk factors Pathogenesis Spectrum Prevention
3. Atherosclerosis is the leading cause of death and disability in the developed and developing world Clinical manifestations depend on the particular vascular bed affected Coronary vasculature angina, MI, sudden death Cerebral TIA, stroke Peripheral claudication, gangrene Renal hypertension
4. Atherothrombotic disease is often a diffuse condition involving multiple vascular beds Multi-territory atherothrombosis 3-8% have symptomatic atherosclerosis in all three territories 23-32% have involvement in two territories
5. Epidemiology Risk factors Pathogenesis Spectrum Prevention
6. Epidemiology Epidemiology The three major clinical manifestations of atherosclerotic CVD are: CHD CVA PVD
7. Disease impact: In 1997, more than 5mn Americans had CVD Currently one in five American has some form of CVD Each year 1mn deaths are due to CVD (42% of all deaths!) One-sixth of CVD deaths are in persons <65 yrs of age Annually 1.5mn Americans have MI 0.5mn die from CHD 0.5mn have stroke 0.15mn die from stroke
8. Death rates from CHD has decreased by 40% since 1968 CVD still remains the leading cause of death in developed nations CHD & stroke are the 2 nd and 3 rd leading causes of mortality even in the developing regions
12. Economic impact: Despite age adjusted decline in CVD mortality, there is paradoxic increase in economic burden due to: 1) aging population causing actual number of CVD cases to remain stable 2) technologic advances causing more aggressive and extensive treatment
14. Epidemiology Risk factors Pathogenesis Spectrum Prevention
15. Concept of risk factors for CAD evolved from prospective epidemiological studies in US and Europe which demonstrated consistent association among characteristics observed at one point of time in apparently healthy individuals and subsequent incidence of CAD in these patients. But, presence of a risk factor does not necessarily imply a direct causal relationship.
16. ATP III classifies Risk factors for CVD into three categories: -Underlying -Major (traditional) -Emerging
17. Underlying risk factors include: Obesity Disinclination to exercise Atherogenic diet
18. Major (traditional risk factors): -Age -Male gender -Dyslipidemia High LDL cholesterol Low HDL cholesterol -DM -HTN -Smoking -Family history of premature CAD in first degree relative
19. Emerging risk factors: -Metabolic syndrome -Triglyceride -Lp(a) -Lp-PLA2 -Fibrinogen -Homocysteine -Urine microalbuminuria/creatinine ratio -Hs CRP -Impaired fasting glucose (100-125 mg/dl per ADA) -Markers of subclinical ASCVD ABI Exercise testing EBCT/MRI Carotid IMT
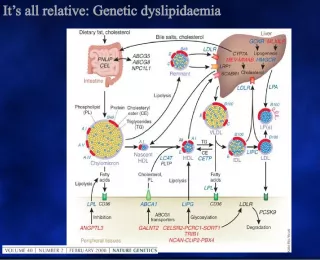
20. Dyslipidemia Dyslipidemia Better term than hyperlipidemia as it includes the risk of having low HDL Serum total cholesterol (TC) is a composite of: LDL cholesterol- directly related to CVD HDL cholesterol- inversely related to CVD VLDL cholesterol- related to CVD in patients with DM and low HDL Best single predictor for CVD risk is TC/HDL ratio. Ideal ratio is <3, intermediate 3-5, high risk >5 This ratio is also the best predictor of treatment benefits
22. Hypertension Hypertension Potent risk factor for all CVD and dominant risk factor for stroke. Graded relationship between level of BP and outcomes. SBP rises with age, whereas DBP plateaus in the late middle life and decreases somewhat then. Trials for isolated systolic hypertension have shown benefits for both stroke and CHD
23. Systolic and diastolic hypertension increase the RR for CVD by 1.6 times For combined Systolic and diastolic HTN the RR is 2.0 The risk for CVD is increased even in individuals with high normal BP (130-39/85-89 mm Hg)
24. Smoking Smoking This habit increases the risk of vascular outcomes by 2 fold. Both, regular and filter cigarettes have same adverse effects. Low tar/low nicotine products have not been shown to reduce the risk Unlike other modifiable risk factors, cigarette smoking can be eliminated entirely Benefits of quitting smoking are dramatic. Risk in ex-smokers falls to near non-smoking levels in 2 yrs.
25. Obesity Obesity It contributes independently to CVD risk and also aggravates known CVD risk factors. Measures of obesity include: BMI Waist: hip ratio.
27. Synergy of risk factors : The CHD death risk in men who smoke, have DBP>90 mm Hg, TC>250 mg/dl, the actual risk is 82/1000 v/s 43/1000 if all the three risk factors are added Thus there is multiplicative effect of multiple risk factors acting in concert. Also control of one risk factor provides substantial benefit in persons with multiple risk factors
29. Diabetes Mellitus Diabetes Mellitus Patients with either type I or type II diabetes have increased risk for CVD Risk of CHD is increased 2-fold in young men and 3-fold in young women with type 2 diabetes Type II diabetics have one or more metabolic abnormalities (hypertriglyceridemia, low HDL, hypertension) They may also have normal LDL levels but LDL particles are dense and small thus being more atherogenic
30. (Circulation 1998;97:1837)
31. Metabolic syndrome: -Abdominal obesity: waist circumference Men >40 inches Women >35 inches -Triglycerides >150 mg/dl -HDL Men <40 mg/dl Women <50 mg/dl -BP >130/85 mm Hg -Fasting glucose >100 mg/dl (presence of 3 or more criteria constitutes metabolic syndrome)
32. Epidemiology Risk factors Pathogenesis Spectrum Prevention
33. Pathogenesis Pathogenesis Atherosclerosis is a progressive disease The term was first proposed by pathologist Felix Marchand in 1904 Athero= gruel/porridge, sclerosis=hardening The process begins in childhood and has clinical manifestations in late adulthood Advanced lesions are a result of three processes: 1. Lipid accumulation 2. Accumulation of intimal SMC, macrophages, T-lymphocytes 3. Formation of connective tissue matrix by proliferated SMC
34. Atherosclerotic disease can lead to stenosis and occlusion as in most muscular arteries or cause ectasia or aneurysm formation as in elastic vessels (aorta) Even in a given arterial bed it tends to involve certain predisposed areas- proximal LAD, proximal renal arteries, carotid bifurcation The process develops over years to decades and progression is not linear and smooth but discontinuous with periods of quiescence and rapid evolution. Manifestations may be varied from asymptomatic to chronic stable angina/claudication to dramatic acute MI/ stroke/sudden death.
35. Normal arterial wall has three layers: intima- limited by internal elastic lamina media- between internal and external elastic lamina adventitia Intima is the site at which the atherosclerotic lesions form Lesions can form in one of the two ways: Positive remodelling- intimal thickening associated with dilatation of the artery, so the lumen remains large Negative remodeling- asymmetrical intimal thickening with lumen encroachment
36. Endothelium: Largest and the most extensive tissue in the body which performs several functions. -Barrier between blood and arterial wall -non-thrombogenic surface by secreting PGI2 -highly active metabolic tissue capable of forming several vasoactive substances and connective tissue macromolecules Endothelial cells have receptor for several molecules: LDL Growth factors Pharmacological agents
37. Initiation of atherosclerosis Lipoprotien accumulation and modification fatty streak formation lipid oxidation nonenzymatic glycation Leukocyte recruitment (T lymphocytes, macro) foam cell formation Evolution and complications SMC involvement
38. LDL Binds to receptor on endothelial cell surface Internalized Oxidized to oxidized-LDL Ingested by Increased adherence Macrophages and migration of T-cells, monocytes from the lumen into the wall Foam Cell
39. Smooth muscle cell Accumulation of SMC in the intima is the sine qua non for atherosclerosis. It proliferates in the intima to form intermediate and advanced lesions of atherosclerosis Smooth muscle cell can exist as contractile phenotype or synthetic phenotype. It is the principal contributor to the reparative and fibroproliferative process in the development of atherosclerosis For the lesions to form, the SMC migrates from the media to intima
40. Vulnerable plaques Thin fibrous cap Large lipid core High macrophage content Stable plaques Thick cap Dense extracellular matrix Less lipid rich core
41. Epidemiology Risk factors Pathogenesis Spectrum Prevention
42. Spectrum of coronary artery disease Silent ischemia Chronic stable angina Acute coronary syndromes Unstable angina NSTEMI STEMI
44. Clinical presentation of CHD depends on age and gender Women: Angina is most common first CHD event followed by MI Men: MI is the most common first event followed by angina. Sudden cardiac death is not uncommon
45. Acute myocardial infarction (AMI) One of the most common diagnosis in hospitalized patients in industrialized nations Mortality of acute MI is 30% and one-half of these deaths occur before hospitalization Mortality after admission has decreased by 30% in last 2 decades 1 in 25 pts (4%) who survive till hospital discharge die within one year
47. Pathophysiology AMI results when thrombus (occlusive/nonocclusive) develops at the site of ruptured plaque Vulnerable plaque Rupture Coagulation cascade platelet adhesion, activation activation,aggregation Fibrin and platelet clot Coronary occlusion MI
49. Amount of myocardial damage depends upon: -territory supplied by the occluded vessel -collateral circulation -duration of occlusion -partial/total occlusion -oxygen demand of jeopardized myocardium
50. Presentation : Chest pain- most common, similar to anginal pain but more severe and prolonged described as severe, crushing/squeezing/pressure worst pain ever Chest pain may be absent in pts with DM or in elderly Atypical presentations: confusion, syncope, profound wkness, arrhythmia
51. Differential diagnosis : Pericarditis Pulmonary embolism Pneumothorax Aortic dissection Esophageal spasm
52. Examination : Anxiety, pallor, restlessness Substernal chest pain with diaphoresis is strongly suggestive of AMI Those with anterior MI may have sympathetic overactivity whereas those with inferior MI may have para- sympathetic overactivity S3/S4 Transient systolic murmur due to dysfunction of mitral apparatus leading to mitral regurgitation
53. Laboratory findings : EKG specific but insensitive tool for diagnosis of myocardial ischemia Total occlusion of infarct related artery leads to ST elevation (STEMI) and subsequent evolution of Q waves Partial occlusion/early recanalization/rich collaterals leads to NSTEMI (non-ST elevation MI)
56. Serum cardiac markers : Released into the circulation from necrotic heart muscle CK (creatine kinase) rises 4-8 hrs after onset of MI and normalize by 48-72 hrs not specific for myocardial necrosis MB isoenzyme of CK is more specific Cardiac specific troponins: more sensitive and specific than CK and CKMB for identification of myocardial necrosis Myoglobin- first serum marker to rise after MI, but lacks specificity.
57. Cardiac imaging 2D echocardiography reveals regional wall motion abnormality also useful to identify mechanical complications of MI Radionuclide imaging used infrequently in the diagnosis of acute MI mainly used to risk stratify patients with CHD
58. Management Prehospital care : Major elements include Recognition of symptoms by the patient and prompt medical attention Rapid deployment of EMS capable of resuscitation and defibrillation Expeditious implementation of reperfusion
59. Goals of Initial management in ED Control of cardiac pain Rapid identification of patients suitable for reperfusion Triage of low risk patients for subsequent care Avoiding inappropriate discharge of patients with MI
60. Aspirin: 160-325 mg chewable aspirin leads to rapid buccal absorption, inhibition of cyclooxygenase in platelets and reduction of TXA2 Oxygen by nasal cannula if hypoxemia is present Sublingual nitroglycerine followed by IV infusion if needed Intravenous betablockers (decrease myocardial oxygen demand, control chest pain and reduce mortality) Morphine for pain relief ( given IV in small doses)
61. STEMI ASA, beta blockers, antithrombin therapy <12 hrs >12 hrs Eligible for Lytic therapy Lytic C/I Not a candidate For reperfusion Persistent symptoms Thrombolysis Primary PCI no yes Other medical therapy Consider reperfusion (ACEI, nitrates, beta blockers, antiplatelets, antithrombin,statins)
62. Time is muscle
66. Door to needle time- 30 min (for patients receiving thrombolytic therapy) Door to balloon time-90 + 30 min (for patients undergoing primary angioplasty)
67. Unstable angina/NSTEMI Aspirin, antithrombin, nitrates, GP IIb-IIIa antagonist Betablockers(calcium channel blockers) Assess clinical status High risk/unstable Stable (Recurrent ischemia, LV dysfunction Widespread EKG changes, positive enzyme markers) Cardiac catheterization Severe ischemia Revascularization (PCI/CABG) Medical therapy Stress test yes no
68. Chronic Stable Angina : Patients with stable angina should undergo detailed evaluation including history, focused physical examination and risk factor assessment Initial laboratory evaluation should include: hemoglobin, fasting glucose, fasting lipid profile EKG and chest x-ray Precipitating factors for angina (anemia, arrhythmias, valvular disease) should be identified and treated
69. Ten important treatment elements of stable angina include: A aspirin and anti-anginals B beta-blockers and blood pressure control C cholesterol and cigarettes D diet and diabetes E education and exercise
70. Patients with intermediate probability of CAD may undergo stress testing for diagnostic and prognostic purpose Patients with high probability of CAD may also undergo stress testing for prognostic purpose Individuals with high risk characteristics on stress testing may proceed with coronary angiography and subsequent revascularisation
71. Epidemiology Risk factors Pathogenesis Spectrum Prevention
72. Prevention: Opportunity for treating the underlying process of atherosclerosis and preventing its acute complications presents enormous challenge and opportunity Prospective community based Framingham heart study provided support for the fact that hyperlipidemia, hypertension and other risk factors correlated with cardiovascular risk Seven countries study provided a link between dietary habits, serum cholesterol and cardiovascular risk
73. Dyslipidemia: It is the most established and best understood risk factor for atherosclerosis. National guidelines recommend cholesterol screening with fasting lipid profile in all adults. Individuals with dyslipidemia should have dietary modification Normal total cholesterol should not reassure individuals having other risk factors or low HDL Primary and secondary prevention trials in individuals with not only high but even average total and LDL cholesterol have shown significant decrease in CHD events by 24-31%.
74. NCEP recommends that target LDL for: Individuals with established CVD/ DM/ estimated 10 yrs risk for CHD events>20% <100mg/dl Individuals with 2 or more risk factors for CAD 100-130 mg/dl Others 130-160 mg/dl
75. Circulation 2004;110:227-239
76. Diabetes mellitus: Diabetic dyslipidemia is characterized by: normal LDL- but more dense and atherogenic low HDL elevated triglycerides Having diabetes places individuals at same risk as those with established CVD Strict glycemic control helps to decrease microvascular complications but not CHD events. However, statin therapy has demonstrated unequivocal benefit in diabetic patients
77. Hypertension: Trials have shown that pharmacologic therapy of HTN reduces the risk of stroke and CHF. But evidence for reduction in coronary events has not been so strong.
78. Smoking cessation: In FHS, smoking was found to increase the risk for CAD, stroke, heart failure, and peripheral vascular disease at all levels of blood pressure Smoking cessation in hypertensive patients who smoke 1 ppd was estimated to reduce cardiovascular risk by 35-40% 2-3 yrs after cessation, the risk for CAD declines to that of subjects who have never smoked
79. Lung Health Study Annals of Internal Med, 2005